
With the connected care and telehealth coverage dependent on COVID-19 public health emergency (PHE) waivers issued in 90-day increments, the key question for 2021 is: What connected care, remote patient monitoring and telehealth policy changes on coverage will become permanent and when will we know?
While there is certainty that COVID-19 PHE waivers that provided broad coverage for connected care and telehealth will remain in effect through 2021 based on the U.S. Health and Human Services letter sent to governors, policy for 2022 and beyond is uncertain. Consistent and persistent connected care and telehealth coverage across major payers will require statutory and regulatory change in 2021.
The impact of the uncertainty of how, when and whether telehealth coverage continues is clear from the utilization data, with telehealth visits increasing dramatically and then lowering to about 6.5% of all healthcare claims. Healthcare providers may be reluctant to invest in the software, equipment and workflow modifications needed to support telehealth without consistent and persistent coverage. Without changes in coverage policy for 2022 and beyond, we would expect telehealth use to contract to a level between the 0.38% of healthcare claims in February of 2020 and the 6.5% of healthcare claims in December of 2020.
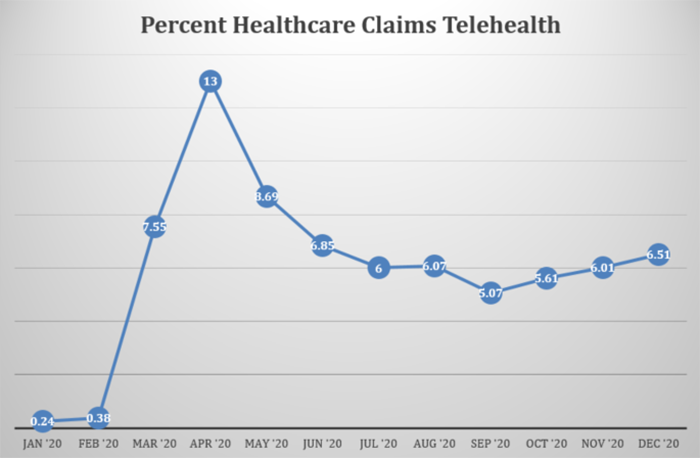
Source: Fair Health, Monthly Regional Telehealth Tracker
Will this year bring clarity for connected care and telehealth policy?
During 2021, we expect a combination of statutory (legislation) and regulatory (agency rulemaking) on Medicare coverage of telehealth and connected care, but we do not expect actions that will make the current waivers permanent on a wholesale basis.
The following are three predictions on connected care and telehealth policy over the year.
1. Congressional and agency staff concerns will lead to policies that include barriers to connected care.
Congressional and agency staff concerns about overbilling, over-use, as well as fraud and abuse combined with misunderstanding of the efficacy and appropriate use of connected care will lead to policies that include barriers to connected care. The policies that will create barriers include:
- Requiring in-person visits prior to delivery of connected care
- Reimbursing connected care at a lower rate
- Prohibiting ancillary providers delivery of telehealth and connected care services even when done under direct supervision of the billing provider
- Covering a much more limited set of telehealth and connected care services for beneficiaries when they are in their home
2. Medicare regulatory policy will adopt new restrictions in the Medicare Physician Fee Schedule.
Medicare regulatory policy on virtual visits or remote physiologic monitoring (defined by Medicare as “NOT telehealth”) will adopt new restrictions in the annual update of the Medicare Physician Fee Schedule. Specifically, it is possible that policies that Centers for Medicare & Medicaid Services will propose to narrow the definition of the monitoring equipment that is eligible to be billed under CPT code 99454—establish specifications on types of physiologic data collection versus clinical status information collection, and possibly add specifications on the clinician time requirements.
3. Congressional action will be narrowly focused.
Congressional action on connected care and telehealth will be narrowly focused and likely to simply extend the waivers through 2022 or 2023, allowing for time to collect data and analysis. With the Medicare Payment Advisory Commission (MedPac) report to Congress recommending an “extension of some telehealth expansions.” The temporary and limited Medicare telehealth expansion seems the most likely route for Congressional action. This means that the waiver extension may only pertain to Medicare telehealth coverage (live audio-visual visits), not to remote patient monitoring or virtual visits. And Congressional action is likely to include one or more policies designed to prevent “over-utilization”. Action will be most likely in the last quarter of 2021 as there is no pressure to act until the PHE is on the verge of expiring.
Share Your Connected Care Data and Experience
Policymakers need to understand how connected care improves the efficacy and quality of care and holds potential for controlling costs. Examples of appropriate use and consumer acceptance will be essential to building support for policy to support and maintain coverage of connected care beyond the COVID-19 PHE. Healthcare providers and healthcare systems must publish in both journals and newsletters how they have used connected care and what it means for their patients and then they must share those publications with their elected officials.
COVID-19 Global Policy Call to Action
HIMSS calls on government, businesses, civil society leaders and elected officials to recognize the important role and value of health information and technology during a health emergency and to work across industries to leverage sound health data, tools of informatics and innovative solutions outlined in our Global Policy Call to Action.



