
HIMSS and PCHAlliance have long envisioned a healthcare system that seamlessly incorporates the use of connected care to enable improved quality, identify measurable outcomes and increase access to healthcare for consumers, while reducing complexity and costs.
Connected care and communication technology-based delivery can improve our healthcare ecosystem by:
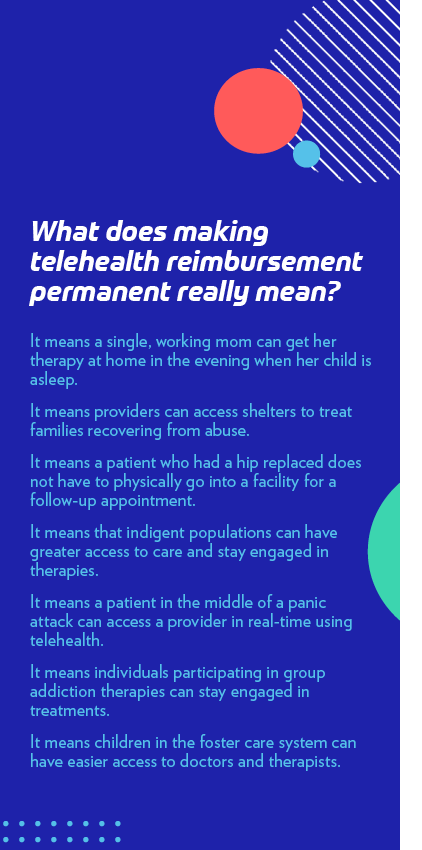
- Expanding access to healthcare by removing many barriers to care created by in office/clinic appointments. Connected care has expanded access to many underserved communities and individuals in ways never before envisioned
- Simplifying the process of navigating healthcare delivery for patients
- Empowering patients and caregivers with self-care and health engagement strategies
- Improving value of healthcare by maintaining or improving care quality with no increase in cost
- Enabling access to mental and behavioral health services, helping address provider shortages by improving efficiencies and stigma that inhibits patients from visiting mental health clinics
- Promoting administrative efficiency, including bi-directional communication using actionable information based on patient need
When the COVID-19 public health emergency (PHE) in the U.S. subsides, the policy waivers, temporary healthcare standards and policies that have been adopted for Medicare, Medicaid, private payers and professional licensure will require a transition—rather than a sudden termination—to ensure stability, embed resiliency and develop a modern, value-based, health delivery system with digital health tools. We believe a framework focused on advancing value-based, patient-centered healthcare should guide the phasing down of some waivers and make others permanent.
Principles to Guide Transition Plan for PHE Waivers
We have identified a set of guiding principles through consultation with subject matter experts in connected care, evidence-based digital health tools and innovation. Those experts uniformly identified telehealth, communication technology-based services and virtual care policy waivers as key for the long-term transition of healthcare delivery to a system that improves care, increases access, reduces complexity and costs, and enables resiliency. Creating a comprehensive policy framework that is predictable, forward-looking, and encourages innovative and novel approaches to care delivery, all while ensuring patient safety, will be critical.
It is vital to retain policy waivers for telehealth, communication technology-based services and remote physiologic monitoring while a principle-based, time-defined process to evaluate the modification and permanence of waivers occurs.
Guiding Principles for Policy to Permit and Incorporate Innovations and Digital Health Tools
- Policies adopted must protect or improve quality, safety and outcomes of care based on available evidence
- Connected care offers different value than in-person care, and as such it should:
- Not be adopted and used exactly as in-person care would be delivered, unless evidence supports adoption and use in such a manner
- Be valued, paid or priced based on the overall value it brings to care delivery
- Policies on connected care should enable and improve safe, reliable access to healthcare regardless of race, ethnicity, age, income, geography, gender, religion, sexual orientation, physical or mental ability, or other socio-economic factors
- Policies should improve access to value-based care for at risk communities, advancing health equity
- Policies must enable coverage of data-driven and evidence-based connected care, which means:
- The best available research evidence shows the service works and leads to appropriate clinical outcomes
- Clinical expertise can be used to evaluate the risks and benefits of a connected care service or tool to deliver care
- Patient and client preferences support use of communication technology-based services and tools
- Policies must be technology agnostic to allow for incorporation of innovation and new evidence-based digital health tools
- Policies must be forward-looking, flexible and adaptable to evolving and future applications of connected care, which would prevent or diminish innovation
- Connected care coverage must be designed to deliver care in ways and means that patients and providers prefer, and in a manner that is most comfortable to them
- In some cases a patient may wish to choose a technology-based tool with less privacy protection; privacy and security cannot be used as excuses to drive market share or limit access to only one connected health tool
- A patient should have the choice to communicate and interact with their provider in their most preferred method, either a telehealth service or an in-person visit
Guiding Principles for the Post-PHE Transition Process for Connected Care Policy Waivers
- A determination to wind down the PHE waivers, should include advance notice of at least 90 days, along with a written plan and timeline made available to the public
- Public comment and feedback should be solicited on the plan and timeline
- The determination to wind down the PHE waivers must be publicly provided and must be based on documentable benchmarks or milestones, such as administration of vaccine to a pre-determined percentage of the population, to give patients and providers assurance that healthcare services are being delivered in the safest possible manner and to provide advanced notice for planning of practice and work flow changes
- The plan should be process-oriented, comprehensive and deliberately developed, including obtaining counsel and support from Congress
- The plan should include a detailed list of which waivers will be made permanent and which will expire, and an explanation of why the determination was made for each
- The process must include a Centers for Medicare & Medicaid Services’ study on how telehealth and other connected care technologies were leveraged in response to COVID-19
Specific Policy Waivers and State Policies That Meet These Guiding Principles
Federal waivers that should become permanent policy:
- Lift originating site restrictions in Medicare:
- “Site of residence” for a patient should be an originating site, to account for alternative living situations and better meet patients where they’re located
- Eliminate Geographic Restrictions for provision of telehealth services
- Allow clinicians to reduce or waive any potential cost-sharing obligations when cost sharing is minimal for telehealth and communication technology-based services
- Currently Office of the Inspector General policy is non-enforcement of cost sharing
- This policy should be made permanent
- Remote Patient Monitoring in Medicare may begin without an in person, face-to-face visit
- Use of audio only in the following cases:
- When accompanied by remote patient monitoring, sharing of patient generated health data, e.g., home blood pressure readings or glucose meter readings
- When patients do not have broadband access
- For services with evidence base showing equal efficacy (counseling or medication adjustment to treat mental health conditions)
- Allow delivery and billing of telehealth services by allied health professionals, e.g., respiratory therapy telehealth services by respiratory therapists and nurses, physical therapy telehealth services by physical therapists
Federal-state coordination and alignment:
- Put in place federal policy and incentives to encourage states to adopt Interstate Medical Licensure Compact and to permit delivery of telehealth by out of state providers
- Encourage and/or incent states to eliminate in-person consent for delivery of telehealth or remote patient monitoring
- Require state review of licensure and connected care coverage policies and laws for healthcare resilience
- Medicaid incentives to include broad incorporation of connected care on a permanent basis, because the capacity needs to be part of the system or it won’t be there next time
- Establish state requirements that state regulated insurance plans must cover connected care, reimbursing at 80% or more of similar in-person care
COVID-19 Experiences and Lessons Learned From the Field
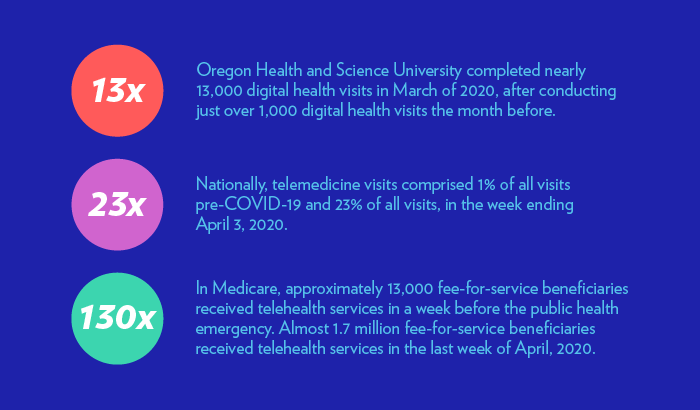
In response to the urgent needs and unique challenges presented by the COVID-19 pandemic, regulatory changes across all levels of government unleashed an unprecedented wave of telehealth and connected care adoption to protect patients and providers and allow communities to adhere to social distancing measures and stay-at-home orders.
As we continue to learn and grow from these experiences, we have witnessed a few common takeaways, lessons learned, and remaining barriers to adoption. Even while expanding access disparities in access have been further highlighted and, in some cases, exacerbated.
Lack of reliable and affordable broadband has continued to prevent many patients and providers from utilizing telehealth, as has lack of access to technologies that can support live voice-video communications or provide real-time or regular tracking of a patient’s physiological data. Work by Health and Human Services and the Federal Communications Commission will be essential to address these barriers.
Workflow and planning are important and there are many lessons on building capability for each and every provider of healthcare—connected care and telehealth cannot and should not be consolidated into a few national providers, rather it must be integrated into provider workflow throughout the healthcare delivery system. Resources exist to provide roadmaps and assistance to clinical practices and hospitals.
COVID-19 Global Policy Call to Action
HIMSS calls on government, businesses, civil society leaders and elected officials to recognize the important role and value of health information and technology during a health emergency and to work across industries to leverage sound health data, tools of informatics and innovative solutions outlined in our Global Policy Call to Action.