
Data is the new solar and a precious asset for any business. In healthcare, it is the very fabric from which smart and evidence-based decisions are made. With the continued expansion of big data, it will become even more important to leverage cognitive and machine learning capabilities and analyze data cohorts. This will help deliver new business models and new insights to improve health outcomes, patient engagement and coordination across the care continuum.
A data-driven, data-rich approach creates huge advantages for healthcare as a whole by supporting data interoperability and collaboration between stakeholders, including those focused on acute care, those working in social care, research institutions and others, such as healthcare payers. Better use of data will also be a primary enabler of three capabilities that affect all stakeholders: smart engagement, the patient journey and 360-degree understanding.
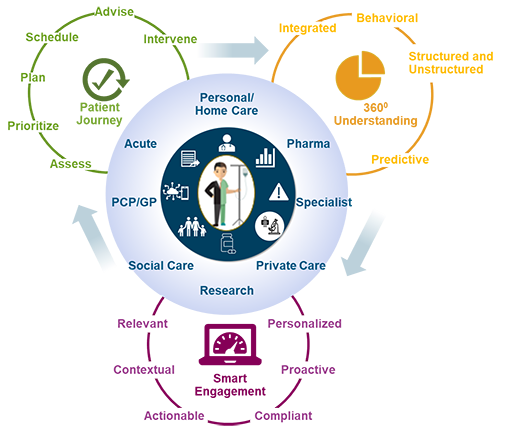
Image source: DXC Technology
Smart engagement is made possible when data is presented in a relevant, personalized and contextual way. Often patients want to be active participants rather than passive recipients of healthcare services, which is made possible by new digital tools that provide them with the insights they need to support and inform them. The patient journey, whether inside or beyond hospital boundaries, must be supported with real-time data to enable both clinical and nonclinical pathways to be coordinated in order to deliver high-quality care. Access to relevant information in real time will help to overcome potential bottlenecks. For example, if the flow of patients through the care journey is delayed, services such as other appointments, cleaning, transportation, meal ordering and others are also pushed back. Real-time data will also enable health intervention before problems occur.
Ultimately, all stakeholders benefit from having access to a 360-degree understanding of all relevant data—clinical as well as nonclinical. To achieve that goal, data will need to be made available and understandable—through standardization—outside of the silos where it was generated. The ability to contextualize the data in the right place, at the right time for the right patient through technologies such as predictive modeling and artificial intelligence will help to support smart engagement, the patient journey and 360-degree understanding.
How, though, do healthcare providers achieve these objectives and pursue a data-driven agenda? Consider these five principles to achieve better data interoperability.
Principle 1: Healthcare Providers Need Access to Data Beyond Silos
One of the big challenges healthcare has often faced is enabling access to data that lies within certain applications, such as EMRs. The data models are often proprietary and if all applications need to have specific interfaces, healthcare organizations must tackle a complex “spaghetti diagram” of interfaces. Once a single change occurs in one system, the interfaces also need to be changed to maintain the flow of data. Furthermore, system-to-system interfaces are often designed for a specific use case, and the risk of them not supporting other use cases is substantial. The integration architecture in these siloed applications is static and cannot adapt to new business changes, such as a move toward telemedicine as a service.
When data is aggregated, standardized and stored in a repository outside of the silos, organizations can leverage that data in different ways. For example, if a patient is affected with a contagious disease and has been on a hospital ward for 12 hours, it is important to know who has been in the room and what equipment has been used and where it is being kept. This will help the staff break the chain of contamination.
To obtain that knowledge, data from various systems, such as the EMR, booking systems, medical equipment databases, as well as data from the real-time location system, must be combined. Using data from one of those systems alone will not provide the whole picture. Furthermore, it means organizations can develop and implement new applications without any disruption to existing solutions.
Principle 2: Healthcare Providers Need Rich Data Interoperability
For the past 20 years, data integration and operability have been defined as sending messages to and from the EMR. New standards offer more seamless data-sharing options and provide a far richer and more impactful set of capabilities. While messages to and from clinical applications still have relevance, data-sharing capabilities that enable true and actionable insights are growing in importance. The new data-sharing models have the potential to transform healthcare by supporting progressive business models such as smart engagement. The ability to share clear, consistent patient data is integral to driving patient-centric care, since patients now demand that healthcare organizations interact with them through multiple communication channels to support the entire healthcare journey.
To get started, hospitals must identify their primary operational challenges and determine which use cases could solve those challenges. Next, they must identify the data that could be leveraged to support the use case and where that data is located. That data will need to be moved outside of the host application and then standardized and ingested into a central repository where it can be accessed in an aggregated form. The exact interface will need to be designed, whether it is a real-time dashboard, a mobile app or maybe even an update to the EMR.
Principle 3: Healthcare Providers Need Real-Time, Actionable Insights
Reports and dashboards have been the norm in many hospitals when talking about business intelligence. But just how relevant is data that is months old, by which time it is difficult to identify the root cause of a problem? Trying to manage a hospital using spreadsheets, dashboards and historical reporting is like driving a car using only the rear-view mirror. You need access to real-time data in order to act immediately and automatically. Access to real-time data will also help you improve operational efficiency, as the data can be used to predict arrival and discharge rates in the emergency department (ED) or potential lack of alignment between resources needed in the immediate future and those available in your current situation.
To gain access to real-time data, you must have established a real-time data feed from your core applications and into your centralized data repository/data lake. When data is ingested into the repository, it can be monitored in real time and specific automated workflows initiated. Such workflows might include sending out an alert or notification if a certain clinical activity has not been conducted as specified by a clinical guideline.
Principle 4: Respond to Challenges with Automated Workflows
Hospitals must make the leap to event-driven and rich-data sharing in healthcare, where data in real time is monitored and intelligent steps can be taken based on the structure or content of the data. These steps, interventions, notifications, alerts or tasks will be initiated based on specific automated workflows the hospital has configured, such as notifying the radiology department to expect a big increase in cases if a large number of patients present to the ED.
The objective is to monitor data for a specific event and then, if it occurs, a workflow is initiated that automatically triggers an action. One example is when an automated guided vehicle arrives with food at the hospital ward (event) and then the system automatically creates a task in a task management system for someone to go get the food (workflow). Another example concerns research. When a referral is sent to the acute hospital, the system will monitor whether it has specific data-matching inclusion criteria for research projects. The workflow engine will then notify relevant researchers about the potential candidate to include in their research project or projects.
Principle 5: Data Must be Shared Using Industry Standards
To achieve full data interoperability, data must be standardized to create uniformity before it is ingested into a central database where clinical data is stored, such as an EMR. This is where a standard, such as FHIR, can transform how healthcare data is used and shared. Healthcare providers get simplified, ubiquitous access to all relevant data that can be shared through a standardized application programming interface gateway.
Moving away from the proprietary format and into the fast lane of data interoperability requires standardization both in data format and semantic standardization or meaning. FHIR consists of a standardized set of resources that can be connected to each other, such as relating all subtypes of diabetes to the main type diabetes. That makes searching easier and helps with pattern recognition. Often vendors will have created a canonical data model with relationships in advance, so the hospital needs to identify only the data elements required to pursue a use case.
The Big Picture of Big Data
As healthcare seeks to create an environment that enables smart engagement, a more connected patient journey and a 360-degree understanding of all the relevant data, adoption of methods, technologies, solutions and standards that will drive those objectives will become paramount.
The views and opinions expressed in this content or by commenters are those of the author and do not necessarily reflect the official policy or position of HIMSS or its affiliates.
Discover the Power of Interoperability
Help advance interoperability and standards-based health IT systems that lead to meaningful health information exchange.



