
Executive Summary
When over 400 clinicians were set up with video visits including: all primary care providers, all specialists, all advanced practitioners, all Gilchrist providers (GBMC’s inpatient and home hospice entity), dietitians in Comprehensive Obesity Management/Bariatric Clinic, speech pathologists in the Dance Voice Center between March 1, 2020 and March 16, 2020, video visit workflows were updated to meet the needs of the Public Health emergency restrictions by:
- Promoting patients to create and activate a MyChart account
- Requiring the scheduling of Video Visits in Epic
- Establishing workflows to assist the increased volume of Video Visits in Epic
Greater Baltimore Medical Center (GBMC) was able to rapidly scale the video visits platform to all ambulatory practices and locations, as evidenced by an increase in volume from 59 telemedicine encounters in February 2020 to 13,436 telemedicine encounters in May 2020, more than a 22,670% increase. Patient satisfaction with video visits remained high as evidenced by >90% positive comments in the patient survey about video visits.
As part of the evolution of the video visit process at GBMC, lessons learned included the gain of appreciation for the rich and valuable virtual connections made with the patients through a video platform. The value of virtual encounters has extended beyond the impetus of extreme social distancing and sheltering in place. Video visits continue to be used as a significant platform to provide healthcare throughout the outpatient care areas, as both clinicians and patients view them as a valuable alternative to face to face encounters. Users, both clinicians and patients, realized that the technology to conduct video visits was not a significant challenge and video visits can be an effective substitution for in-office appointments. Organizational leaders discovered that there was an alternative way to engage patients and deliver high-quality care as a response to the public health emergency, but also ongoing as a routine part of delivery of care. Institutional opportunities for improvement related to the need for redundancy of software platforms became apparent when a cyber-event in December 2020 prevented the use of our main Epic integrated video software.
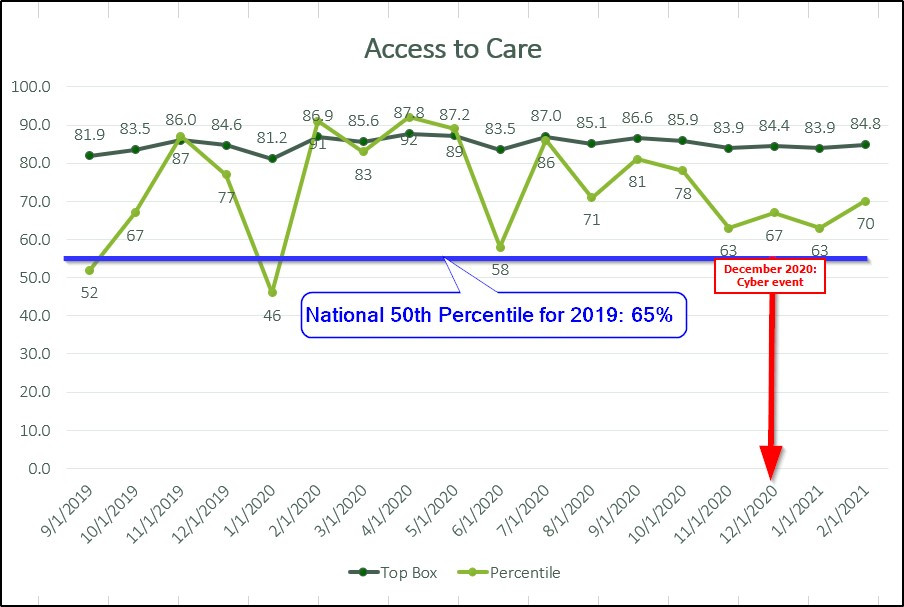
Define the Clinical Problem and Pre-Implementation Performance
GBMC built the necessary framework and implemented video visits for primary care practices as part of a population health initiative in September 2019. Having no prior baseline data for telehealth encounter type, goals were initially set to have each lead provider complete 1 video visit per month to provide feedback on the process and to ensure that the workflow captured all the necessary elements to meet billing requirements. Patient satisfaction was a key performance indicator, and, as such, GBMC set a baseline goal to maintain the current greater than 90% patient satisfaction rate measured by a follow-up survey delivered in the patient’s MyChart account. Lastly, we sought to improve our overall Access to Care rating measured by the Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey domain to 84% by the end of fiscal year June 30, 2020. Patients being seen for anxiety or depression were expected to have completed Patient Health Questionnaire-9 (PHQ-9) or General Anxiety Disorder-7 (GAD-7) screenings using either patient-entered questionnaires in advance of the visit, verified by staff and incorporated into the encounter, or completed with the provider as part of the visit. Visit diagnoses initially targeted were those in which physical assessments were not typically indicated, such as follow-up visits for ADHD/ADD, depression and anxiety. Initial clinician end-users were selected for participation based on their roles as Primary Care Lead Providers, representative of each primary care practice location. Additional providers were added after repeated Plan-Do-Study-Act (PDSA) cycles identified appropriate candidates and adequate in-office support to grow the program. Epic support staff were on hand for each providers’ initial video visit and all offices were provided dedicated iPads to ensure the availability of properly provisioned technology, although many providers with iOS devices chose to use their personal devices. The initial patient cohort was limited to patients insured by CareFirst and GBMC employees covered under our employer health insurance (patient denominators), selected because those insurance instruments represented a known reimbursement model for telehealth encounters. Our initial provider denominator was the cohort of 10 lead providers, and numerator counts included successfully completed video visits conducted by each provider.
Adoption of video visits, according to usage data, was very limited in the pilot study. In February 2020, there were only 59 video visits across all primary care locations. Patients’ feedback indicated that video visit encounters were desired, especially for college students being seen for medication refill reasons, as the patient could be seen regardless of geographic location and distance from GBMC. Access to Care scores noted improvements, too, but with so few appointments being video visits, this increase could not be attributed to patients’ perceived availability of appointments. While recognizing the high satisfaction rate of the video visit option for patients and noting that the average number of lead days between scheduling and encounter occurrence was dropping, clinician reluctance was the barrier in the use of video visits as a key opportunity to provide quality technologically advanced care.

Source: Greater Baltimore Medical Center
Design and Implementation Model Practices and Governance
In compliance with Maryland’s shelter in place orders beginning in mid-March 2020, the GBMC Executive Leadership team fully supported the rapid expansion of video visits to include all clinicians (including advanced practitioners) in all outpatient environments (primary and specialty care) be implemented on March 16, 2020, a lead time of approximately 12 days. The Operations Revenue team would continuously monitor Centers for Medicare & Medicaid Services (CMS) communications for expanded roles and specialties covered under the federal government’s pandemic response, authorizing additional clinical provider types as changes occurred. Lead Providers in the primary care settings who had completed video visits as part of the pilot project were tasked with rapidly training their colleagues within their respective office locations. Epic Physician Champions were tasked with providing training to specialty providers in the specialty outpatient areas, using training material previously created for primary care by the Epic analysts. The Epic Ambulatory, MyChart, and Haiku-Canto analysts were charged with expanding build to adapt to all outpatient specialties, using a single Telemedicine visit type and unified encounter navigator for standardized work and documentation processes. Daily huddles scheduled each weekday morning included the Epic Ambulatory Manager and Team Lead, tasked with coordinating the overarching video visit response, the outpatient Epic Physician Champion, who pooled and triaged all clinical feedback for review and issue resolution, the Haiku-Canto analyst responsible for changes to end-user security, the Ambulatory-MyChart analyst responsible for the build changes, and Epic Ambulatory trainers, who would provide immediate responses to troubleshoot issues as they arose. As CMS identified additional areas of coverage, the Epic analysts added affected user roles to the existing build in a layered approach, testing each role systematically in an end-to-end workflow to make sure hard stops for billing requirements were hit or bypassed as needed per user. Using this method, new areas of documentation were identified as missing from the workflow, such as ophthalmology documentation tools, and the workflows for documentation of screenings previously completed by medical assistants (MAs). As the number of patient encounters completed by video visits reached their peak in May 2020, MAs were incorporated into the standard telehealth visit workflow to ensure medication and allergy lists were updated, specific vitals were recorded, such as weights in our Bariatrics location, and to provide patient communication if visits were running long.
Clinical Transformation enabled through Information and Technology
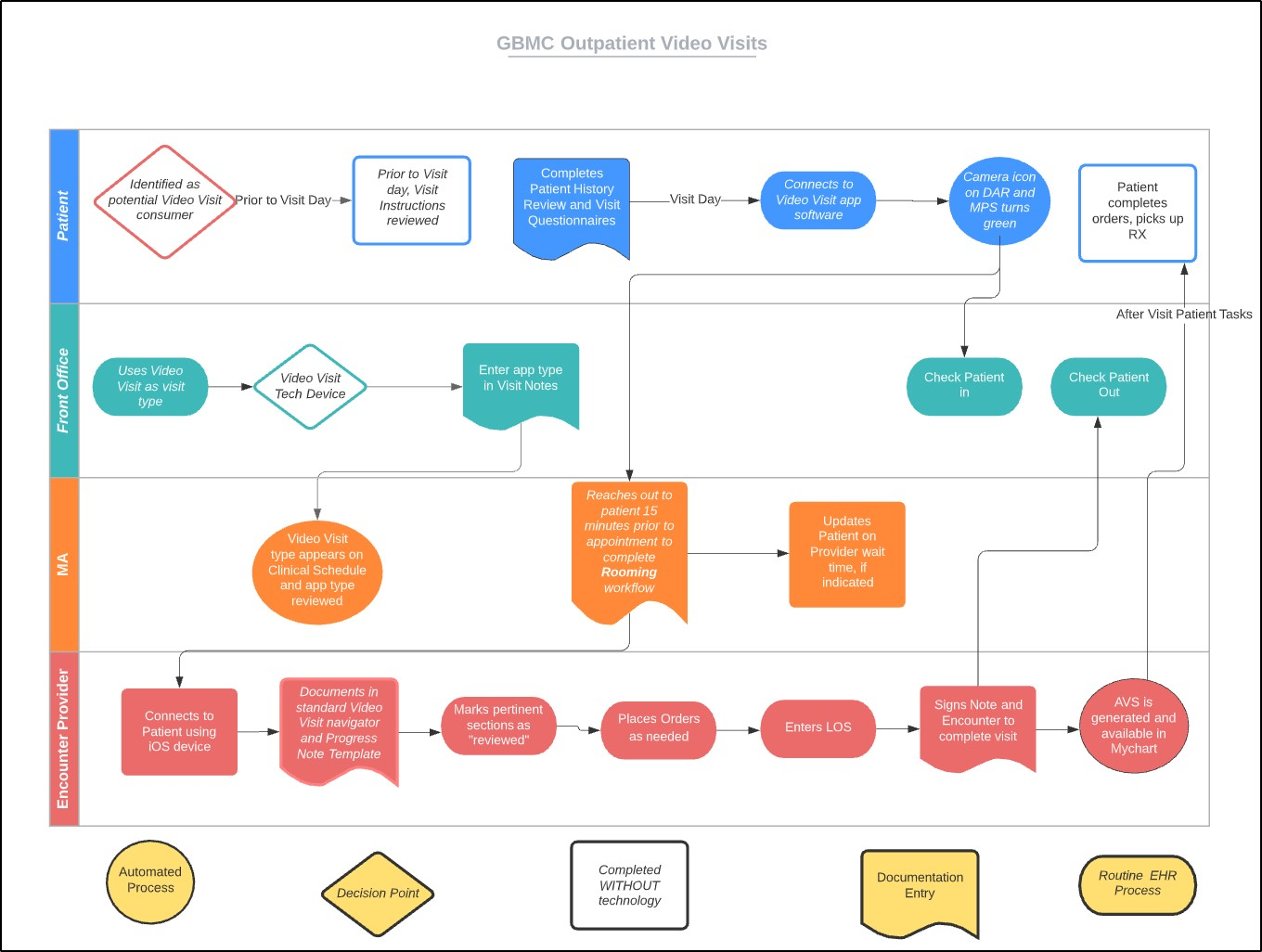
Source: Greater Baltimore Medical Center
Video Visit process from scheduling through completion of patient after visit tasks. By nature, Video Visits rely extensively on technology to produce a successful encounter. In addition to the automation provided by the EHR and the technology to connect the patient to the healthcare system, there are four key participants in a telehealth encounter. First, the patient is at the center of the visit and ensuring this participant could complete the steps required for initiation of the video visit was essential. Our training team worked collaboratively to develop patient-centered instructions, engaging operational users and the Patient Advisory Council to solicit feedback prior to publishing tip sheets for use for the September 2019 go-live deadline. Initial feedback from technology savvy patients recommended a checklist approach over detailed instructions, increasing the likelihood that patients would review the materials provided prior to their appointments.
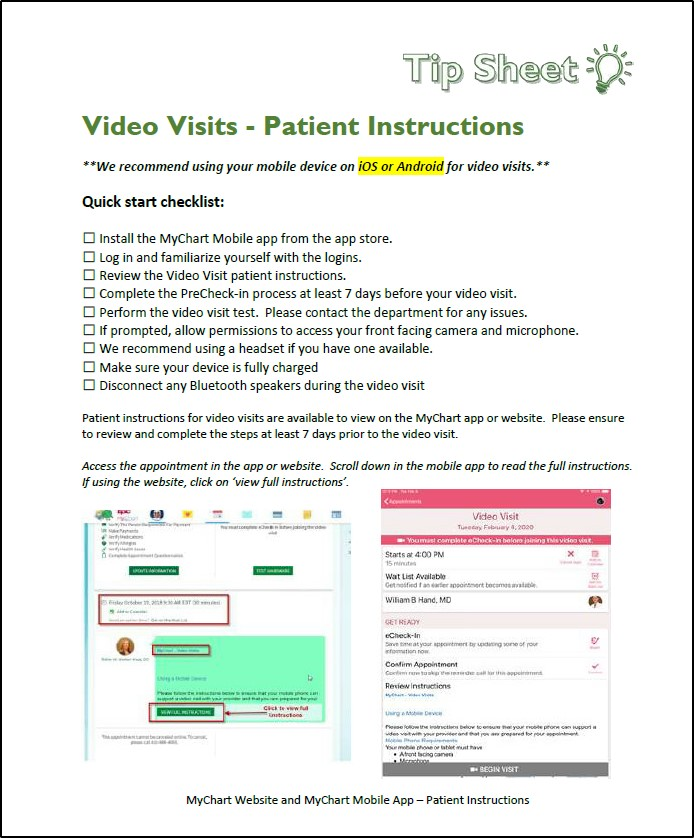
Source: Greater Baltimore Medical Center
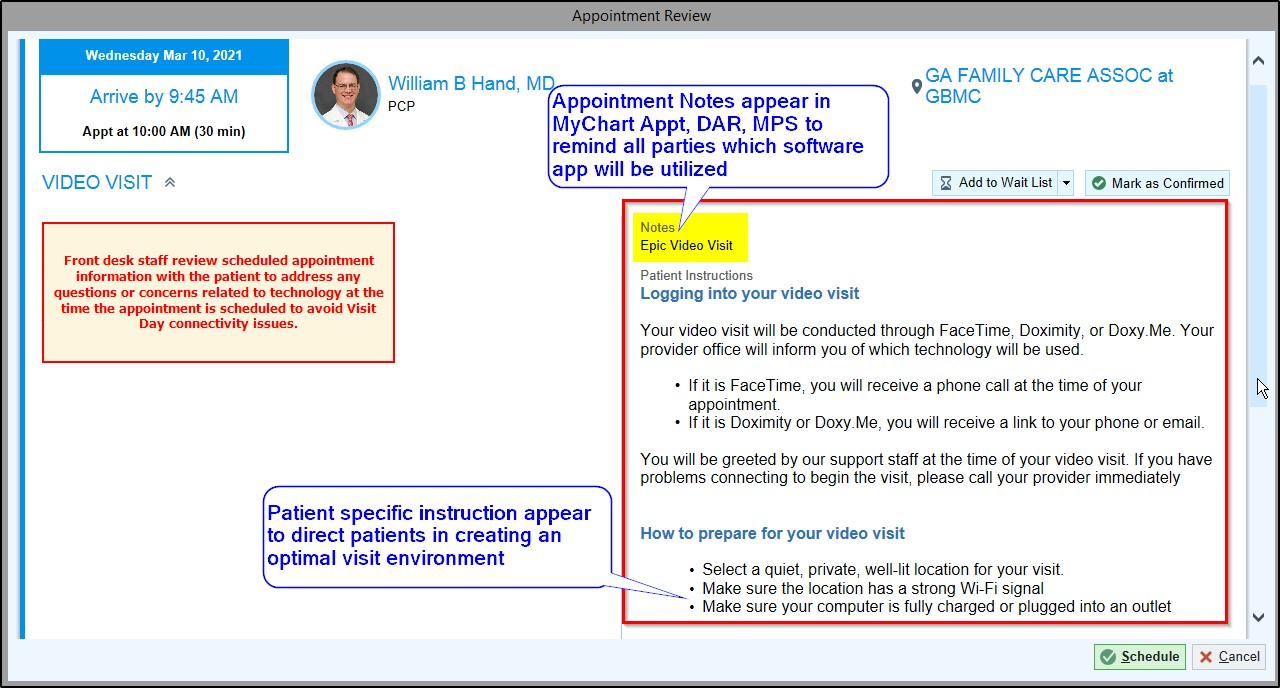
Second, front desk staff were provided targeted instructions within their workflows, in addition to their traditional learning resources. By automatically pulling in the Patient Instructions into the Appointment Review screen, front desk staff were prompted to remind patients which software application was to be used in their encounter.
Source: Greater Baltimore Medical Center
Third, MAs were added to the process as part of the COVID-19 ramp-up. This allowed routine visit documentation such as screening assessments, medication and allergy review, and updates to patient histories to occur as they normally would during an in-person visit. This both reduced the burden on providers and allowed technical assessment and correction of any connectivity issues prior to provider interactions with the patient.
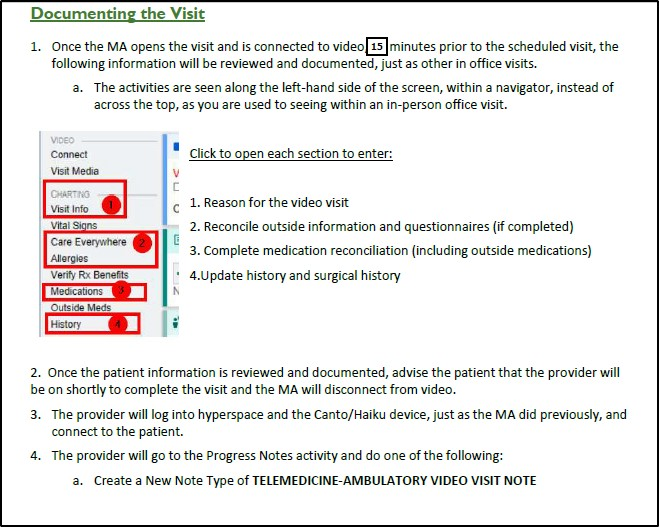
Source: Greater Baltimore Medical Center
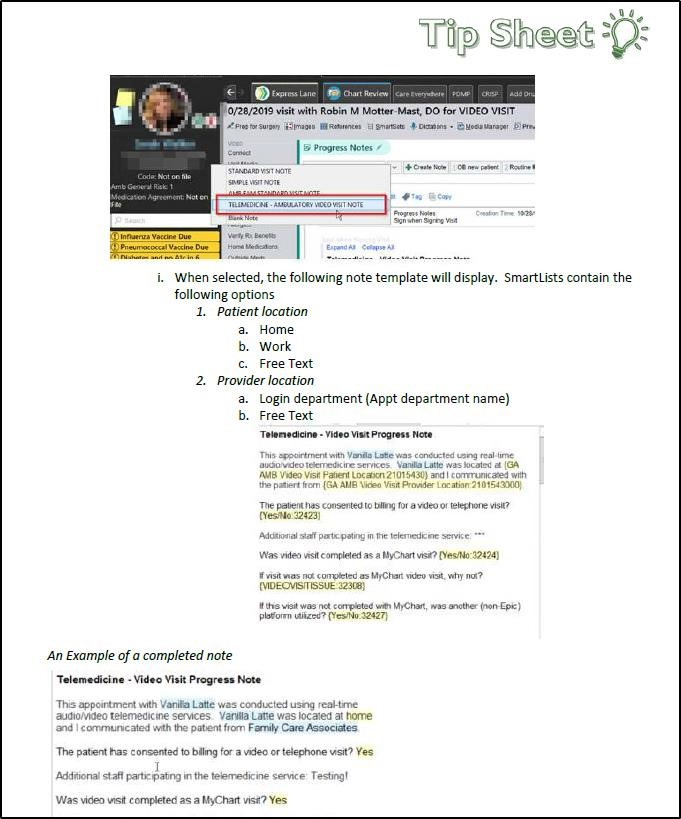
The fourth participant was the encounter provider. As a precursor to system-wide rollout, a single-page video visit tip sheet was created to help guide providers to the key areas of the chart that were required to be addressed to ensure capture of encounter quality metrics and reimbursement requirements.
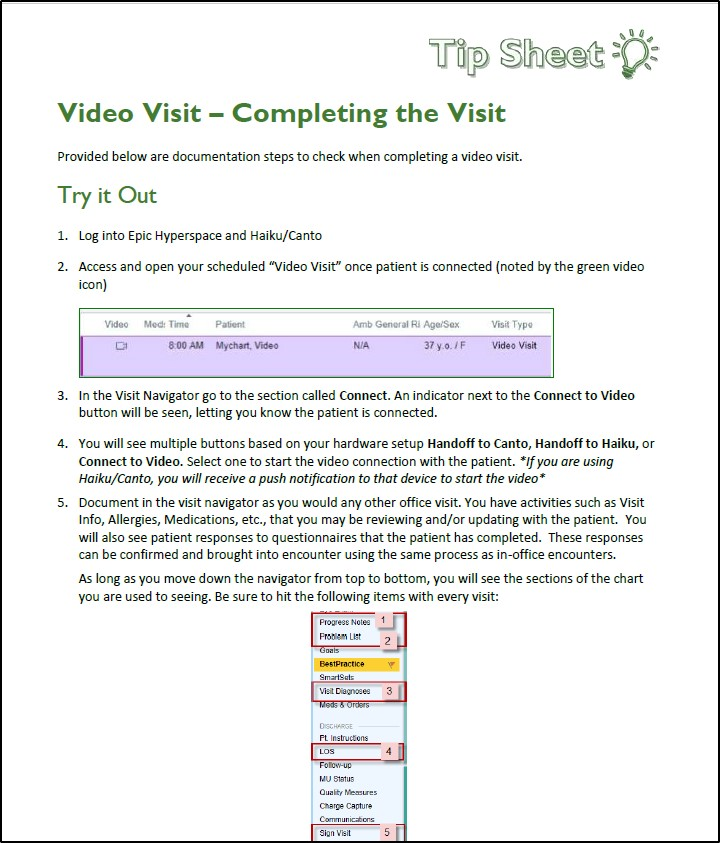
Source: Greater Baltimore Medical Center
The use of a single navigator and standard telemedicine progress note template allowed GBMC to support the needs of all providers, ensuring uniform access to resources, safeguarding accurate documentation of the encounter and proper coding for reimbursement. By maintaining standard work, troubleshooting issues were able to be quickly resolved by Epic Certified Trainers in a centralized support call center. The platform was continuously enhanced and upgraded as necessary and as opportunities for improvement were identified. For example, as additional feedback from the revenue team was received, fields for ‘start of visit time’ and ‘end of visit time’ were added to the standard note template quickly and without the need for additional training.
Source: Greater Baltimore Medical Center
Improving Adherence to the Standard of Care
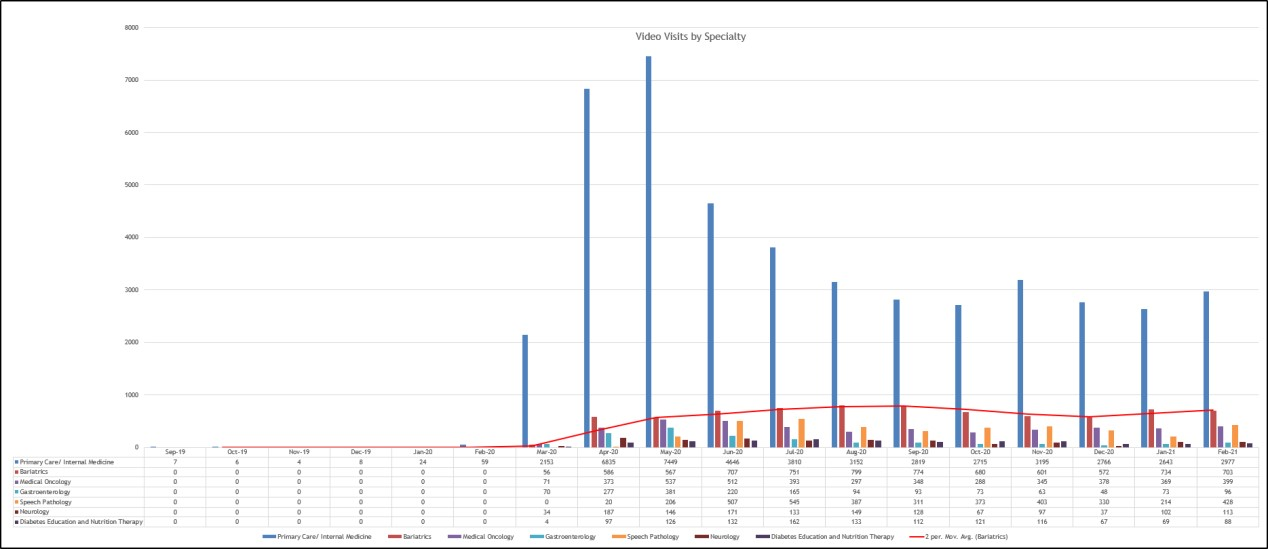
Prior to the COVID-19 pandemic, GBMC recognized the need for video visit encounters to expand the excellent care options available in our primary care locations. In September 2019, we identified a preliminary pool of potential denominator patients as those using either CareFirst payors or GBMC insured employees, who would be undergoing routine surveillance care for a diagnosis of anxiety, depression, or ADD/ADHD in primary care locations. For the pilot study, our numerator population would include patients who had required the PHQ-9 or GAD-7 screenings documented as part of a closed video visit encounter conducted by one of our lead primary care providers. In the six months following the initial go-live date, less than 100 total encounters had been completed, although patient satisfaction reports were noted to be above the 90% approval threshold. The success of the pilot project was establishing the necessary framework for video visits across all primary care practices with high patient satisfaction rates. This allowed for rapid scaling of the video visit framework to address the restricted access circumstances of the pandemic. Following a rapid scaling and expansion of the telehealth platform, GBMC’s pandemic response resulted in an average of 530 video visits every weekday in May 2020, across 32 different specialties and for over 175 different chief complaints. This was an increase in volume of over 22,670%. In October 2020, the Centers for Disease Control and Prevention noted an average of a 50% increase in the first quarter of 2020 for telemedicine visits and 154% increase in video visits across the country for the final week of March 2020, directly related to the COVID-19 pandemic (Koonin et al., 2020). By October 2020, nationally video visits were 67% above pre-pandemic values. While this provides some comparison data points, the very limited usage of video visits at GBMC prior to the pandemic artificially depresses the baseline benchmark data limiting the accuracy of comparison values. In December 2020 video visit encounters had to be backfilled as part of a recovery process resulting from a cyber-event. As an indicator of the popularity of video visits, telehealth encounter volume in December 2020 did decrease by approximately 1,000 total visits, but have shown recovery to the usual monthly baseline as of February 2021, despite Epic MyChart video visits not being available as a result of the cyber event. This is significant because it highlights the need for redundancy of software applications for video visits. As of the end of February 2021, GBMC continues to average over 270 weekday appointments, an increase over February 2020 by 9,200%. Just as important, video visits are now conducted for an ever expanding, wide-ranging, list of indications and diagnoses.
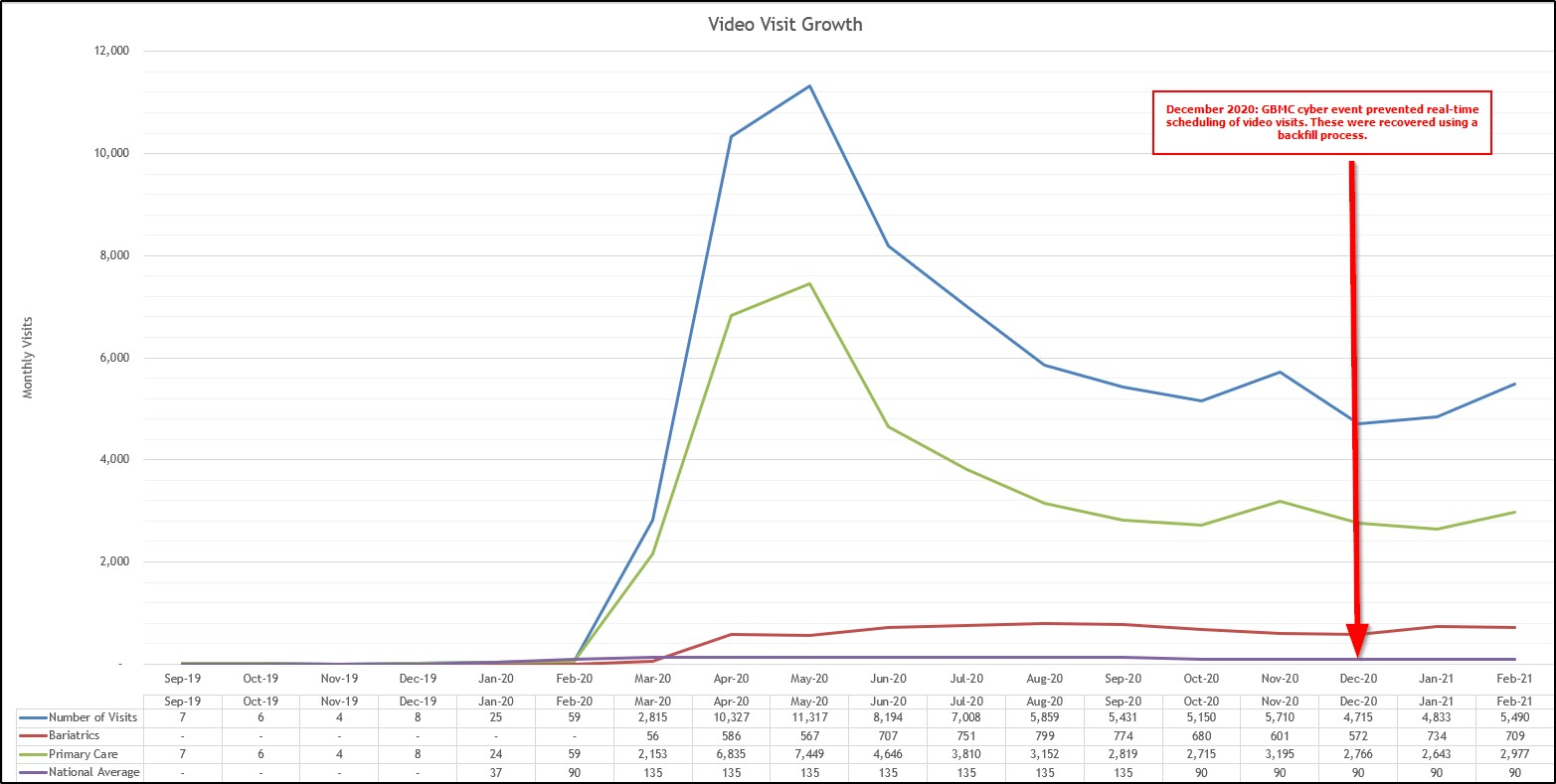
Source: Greater Baltimore Medical Center
In addition to the maintained volume of video visits at GBMC, over 25 specialty departments continue to use and appreciate the flexibility of video visits. Our medical oncology and speech pathology departments have widely adopted this visit type, both averaging several hundred encounters per month.
Improving Patient Outcomes
By the end of March 2020, over 2,800 video visits had been completed across 25 different specialties, quite a jump from the previous month’s 59 visits limited to primary care. As a commitment to quality care and reimbursement, the Centers for Medicare & Medicaid Services (CMS) provided guidance on the coverage of telemedicine encounters across the country (2020). By creating an EHR and technology-based platform that involved patients, office staff and clinicians, GBMC was able to quickly ramp up a previously stuttering video visit care process. While noting primary care represents the bulk of video visits, it is significant to highlight the success of GBMC’s Comprehensive Obesity Management Program (COMP) which has embraced the virtual revolution by committing to 100% virtual care, excluding only day of surgery! This has served to markedly improve access to services for patients previously limited by distance, time, and personal care barriers (GBMC, 2021). Recognized by the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP), COMP serves our patients virtually with scheduled registered dietician appointments, virtual education, bariatric support groups, and post-operative medical weight loss programs for those who struggle following surgery. As a benchmark of success, GBMC COMP monthly visit volumes have remained consistent since June 2020, the first full month of 100% virtual interactions.
While recent studies have noted that many patients missed or delayed preventative screenings, GBMC noted a much better success rate for continued excellence in completing screenings and diagnosing new cancers when compared to our national and international colleagues. Noted in our MDTB presentation, the United States overall had a decrease of 46.4% for initial cancer diagnoses, related to the impact of the COVID-19 pandemic on patients’ access to and consumption of healthcare. The decline in diagnoses was also found in the Netherlands, where a 40% decline was noted, and the United Kingdom which experienced a 75% drop in referrals of suspected cancer (Kaufman et al., 2020).
We believe our success can be linked to video visits, as the primary care team actively targeted patients due for Medicare Wellness Visits as key opportunities for video visits. These wellness visits are not required to include physical exams and are more focused on preventative care. Throughout the visit, discussions on the importance of screenings are had between the patient and provider. Patients and providers were able to use the video visit time to review current care gap status and weigh the risk-benefit ratio for obtaining exams at external diagnostic centers. During Medicare Wellness Visits, the use of Cologuard screening for low-risk patients was actively encouraged by providers, to reduce risks of missed screenings while our outpatient procedure areas were closed pending surge expectations. Colorectal cancer screening metrics from primary care showed that the availability of at-home Cologuard screenings improved performance 3% from a baseline of 70% to a post-implementation rate of 73% during the peak COVID-19 period, which continues to be sustained. Providers also spoke to the safety of accessing mammogram exams in outpatient radiology locations during these visits to ensure continued screening occurred. Breast cancer screening completion has shown continued solid performance, which is better than our colleagues who have noted decreases in mammogram numbers. GBMC noted a 1% increase for completion of mammograms during the pandemic, from a pre-implementation rate of 76% to a post-implementation rate of 77%.
To measure a specialty agnostic metric, GBMC monitored our metric related to the maintenance of an up-to-date medication list throughout our outpatient care areas. We noted a temporary drop in the up-to-date medication list when moving to provider-initiated video visits in April 2020. In May 2020, we incorporated the MA office visit workflow into the video visits to counteract the increased demand on providers and noted a return to baseline in this metric that continues to be sustained. The shared standardized work of the provider-MA medication reconciliation process showed a steady rate of completion at 86.85% prior to implementation and an 86.44% post-implementation rate.
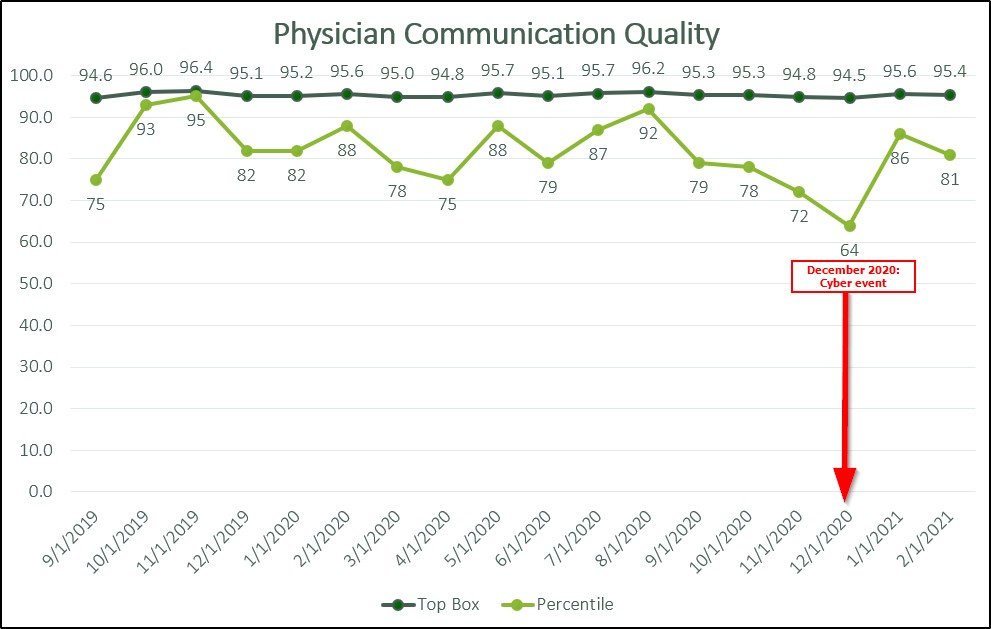
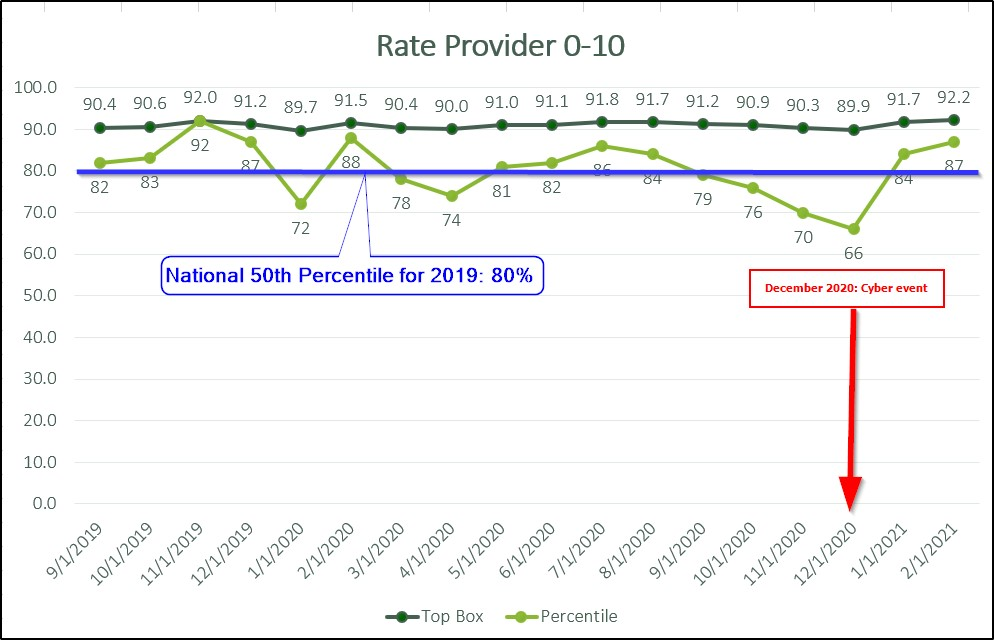
One sentence that encapsulates the 85% GBMC telehealth experience as a whole: video visits were paramount in keeping GBMC’s ambulatory practices open, accessible and moving forward during COVID-19, giving them the ability to serve their population. This is reflected in CAHPS survey information in which GBMC’s Top Box scores consistently exceeded our end-of-fiscal-year goal of 83% during the early COVID-19 pandemic, since few in-office visits contributed to this outcome. Of equal importance and additional significance, GBMC maintained our high expectation for CAHPS score associated with quality of provider communication, with scores consistently above 94%.
Source: Greater Baltimore Medical Center
Source: Greater Baltimore Medical Center
Source: Greater Baltimore Medical Center
Source: Greater Baltimore Medical Center
Accountability and Driving Resilient Care Redesign
During the initial primary care pilot, maintaining high completion rates for reconciliation of medication lists, allergies, problem lists and immunizations was incorporated into all provider led encounters to meet MIPS requirements. The multi-provider schedule (MPS) was redesigned to incorporate visual reminders for both provider and MA highlighting areas needing review through the real-time, system driven report column Outstanding Reconciliation. As clinicians interacted with the areas of the chart mapped to MIPS metric areas, the column would automatically be updated by removing the reviewed area, ending with a blank entry in the column when all sections were properly reconciled.
Adding the column Video helped clinicians recognize when patients were connected to the video visit; the video camera icon would update to a “Green for Go” indicator color when the patient was connected and ready for the clinician to begin the face to face portion of the telehealth encounter. As a real-time requirement, the GBMC Revenue team required all encounters to be closed within 24-hours of completion. By monitoring these areas, GBMC has maintained steady MIPS scores and billing revenue for telehealth encounters.
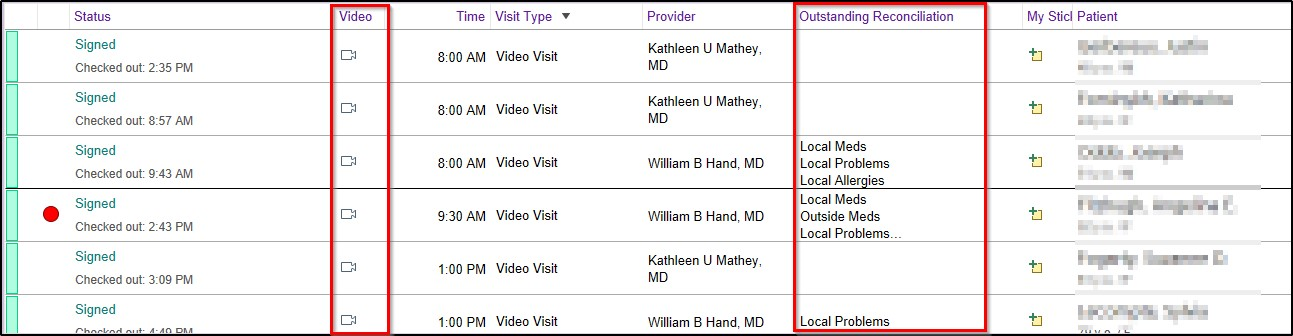
Source: Greater Baltimore Medical Center
References
- Centers for Medicare & Medicaid Services (CMS). (2020). Medicare telemedicine health care provider fact sheet. Retrieved on March 9, 2021 from https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-c….
- Greater Baltimore Medical Center. (2021). Virtual Visit Tips. Retrieved on March 9, 2021from https://www.gbmc.org/comp-vvtips.
- Kaufman HW, Chen Z, Niles J, Fesko Y. (2020). Changes in the number of US patients with newly identified cancer before and during the coronavirus disease 2019 (COVID-19) pandemic. The Journal of the American Medical Association Network Open.3(8): e2017267. doi:10.1001/jamanetworkopen.2020.17267
- Koonin, L. M., Hoots, B., Tsang, C. A., Leroy, Z., Farris, K., Jolly, B., Antall, P., McCabe, B., Zekis, C. B., Tong, I., Harris, A. M. (2020). Trends in the use of telehealth during the emergence of the Covid-19 Pandemic — United States, January–March 2020. Morbidity and Mortality Weekly Report, 69(43), 1595-1599. doi:10.15585/mmwr.mm6943a3.
The views and opinions expressed in this content or by commenters are those of the author and do not necessarily reflect the official policy or position of HIMSS or its affiliates.
HIMSS Davies Awards
The HIMSS Davies Award recognizes the thoughtful application of health information and technology to substantially improve clinical care delivery, patient outcomes and population health.



