
Executive Summary
One of every three patients who dies in the hospital has sepsis. The life-threatening response to infection is difficult to detect in its earliest stages, and every hour that the condition goes untreated increases a patient's mortality risk by 4%. After implementing a rapid response solution in February 2017, teams at the University of Missouri Health (MU Health Care) and the Tiger Institute focused on turning early detection into prompt action. Their work helped increase proactive intervention from the organization’s rapid response team (RRT) — the Tiger Team — while reducing sepsis mortality rates and decreasing code blue calls to resuscitate patients. The patients with sepsis were the first population studied, and the outcomes for overall patient mortality were added as the process matured. The teams also configured IT solutions to automatically calculate each patient's national early warning score (NEWS) and help care teams follow MU Health Care’s NEWS-driven nursing protocol. NEWS summarizes a patient's risk for clinical decline based on commonly tracked vital signs. The higher the NEWS, the more serious the patient's condition. For example, staff were able to reduce the sepsis mortality index by 22% and avoided an estimated 12 sepsis-related deaths within the first nine months of the solution going live. This cannot be solely attributed to NEWS and rapid response, but they are major factors. By using NEWS as the initial warning for clinical decline in all disease groups, frontline staff have been able to get the right attention to the right patient at the right time. Overall, the MU Health Care team saw an increase in rapid response calls, a decrease in code blue calls and an overall improvement in severity adjusted mortality. The initiative was governed through the Center of Clinical Effectiveness and supported through the MU Health Care MIC (Multidisciplinary Informatics Committee).
Lessons learned include:
- It was beneficial to roll out the rapid response solution with the NEWS scores and alerts in phases. By having the algorithms run initially in silent mode, we were able to work with clinicians to make the NEWS and recently implemented Pediatric Early Warning Score (PEWS) as accurate as we could. This helped to ensure the clinicians trusted the scores and were familiar with how they were generated before we went live with the alerting.
- We strongly recommend that any facility pursuing a sepsis identification/alerting system also invest in a rapid response solution at the same time. While it is important to know which patients become septic, early recognition and intervention are absolutely critical and are the key to a successful and comprehensive solution.
- We also found it tremendously beneficial to use the rapid response solution and the structure and standardization it provides to assist in the development of a nursing protocol and sepsis differential diagnosis tool.
- Empower your nursing staff to address the time critical nature of sepsis proactively. The subtle signs of clinical decline are brought to their attention earlier now, and they have been given the tools, support and autonomy they need to provide their patients with the optimal care.
- The nursing protocol is an essential component of success.
- Be patient as you work through adoption. Change management doesn’t happen overnight.
Define the Clinical Problem and Pre-Implementation Performance
Prioritization of the project was based on the importance of recognizing early deterioration in patients’ conditions. For example, in sepsis, one of every three patients who dies in the hospital has sepsis. The life-threatening response to infection is difficult to detect in its earliest stages, and every hour the condition goes untreated increases a patient's mortality risk by 4%. Studies show that early detection and rapid response intervention can have a positive impact on sepsis, as well as other patient conditions in which a code blue or total cardiac and/or respiratory arrest are avoided. Currently, the University of Missouri Health System — with five hospitals with 602 beds in total — is using three EHR provider-based technologies to better identify and treat sepsis: 1) The St. John Sepsis Agent/Sepsis Advisor 2) A Pediatric Sepsis Algorithms and 3) the Rapid Response tool. By comparing actual sepsis mortality to projections based on pre-implementation mortality rates, MU Health Care estimates NEWS and NEWS-driven nursing protocol helped avoid 12 sepsis-related deaths in nine months. University Hospital’s mortality index — a ratio of observed deaths to expected deaths, given the severity of septic patients’ primary diagnoses and comorbidities — dropped 22% during that time.
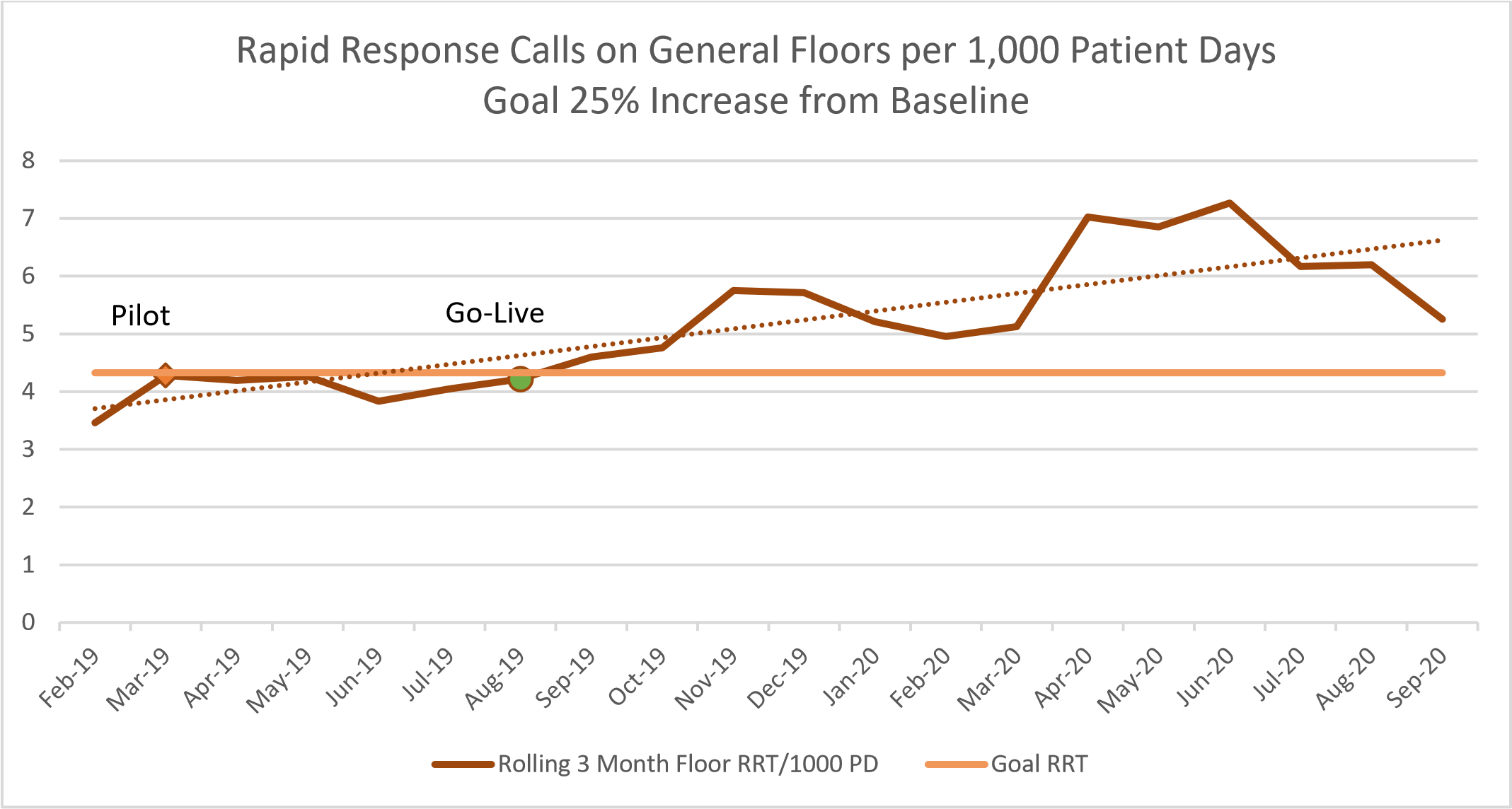
Since MU Health Care turned on the NEWS alerts at University Hospital in August 2019 (100% of patients have a generated score), rapid response calls increased 63% and code blue calls decreased 40%. The overall patient mortality baseline was 0.92, with a goal of the top quartile when compared to other Vizient Academic Medical Centers (0.8). However, in using the NEWS algorithm, MU Health Care has been able to achieve a sustained mortality rate near 0.60 for several months. MU Health Care participates with Vizient, which provides the benchmark data and supplies quality data submissions to CMS.
In the overall outcomes data, the denominator is every patient with a NEWS/PEWS score (100% of in-patients are scored), and the numerator is the patient population with a rapid response or a code blue call, and the sepsis data includes patients with a diagnosis of sepsis. Comfort care patients are excluded.
Design and Implementation Model Practices and Governance
When MU Health Care’s leaders considered additional ways to attack sepsis with a NEWS alert system, they engaged a group of doctors and nurses and members of the Tiger Institute for Health Innovation for their input and ideas. The Tiger Institute is the IT team created 12 years ago as a partnership between their healthcare information technology provider and the University of Missouri.
The history behind the sepsis algorithm and countless other IT innovations dates back to the fall of 2009. That’s when the University of Missouri created a partnership with its health information technology provider. The goal was to become one of the country’s most technologically advanced hospital systems. In 2014, just five years into the partnership, MU Health Care became the first academic health system in the nation to meet the federal government’s standard for “meaningful use” of medical information technology. The teams have accomplished Stage 7 validations in both the EMRAM and O-EMRAM models, along with the achievement of a HIMSS Davies Award. MU Health Care considers one of its most outstanding successes to be the work that’s accomplished through their healthcare informatics teams. When the Tiger Institute began, its first big job was to connect all of MU Health Care’s hospitals and clinics with an electronic health record. Now, the Tiger Institute finds ways to use the EHR as not just a medical record but also a tool to improve patient care.
For the NEWS project, MU Health Care teams analyzed historical patients’ scores to identify when patients typically require RRT intervention or transfer to the intensive care unit (ICU). Guided by those thresholds, they developed an algorithm and a NEWS-driven nursing protocol to help caregivers act appropriately based on the patient’s status and location within the hospital. The score actually ran in the background for two years of development prior to being released to the live domains.
The NEWS Leadership Group, as part of the Tiger Institute, followed the structure of interdisciplinary involvement common to Tiger projects; The Executive Director of the project was the Director of the Lab/Pharmacy; Nursing Managers; Emergency Department Manager; the Medical Director of the MICU and Pulmonary Service Lines; and the healthcare informatics team. The progression of development was turned over to the NEWS Hardwiring Group, which meets as needed to continue to refine the process. As the project continues to mature, it will be turned over to the Clinical Decline Committee. Operational maintenance is based on: Multidisciplinary Committees, are function focused and with a shared leadership structure based on the Plan, Do, Study, Act process.
Education was driven by nursing leaders who fostered success by educating their teams on NEWS and related nursing protocols during brief, timely pre-shift huddles. As the project continued, nursing huddles reinforced NEWS’s importance by celebrating successful patient outcomes. There were also educational sessions for the residents and physicians. All sessions included the science behind the algorithms, the changes to the visuals for alerting withing the workflows (EHRs, Dashboards, etc.), the process of alert monitoring to minimize alert fatigue and resources available to answer any questions. The training sessions progressed as rolling education to keep teams up-to-speed as improvements and changes were made.
Clinical Transformation enabled through Information and Technology
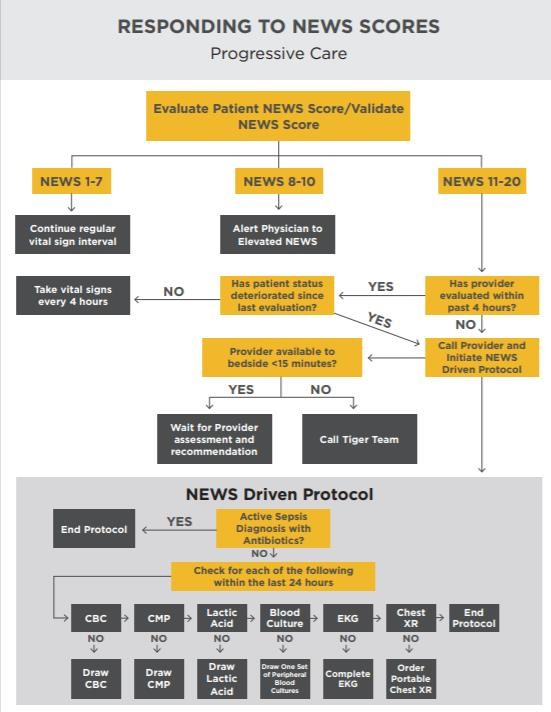
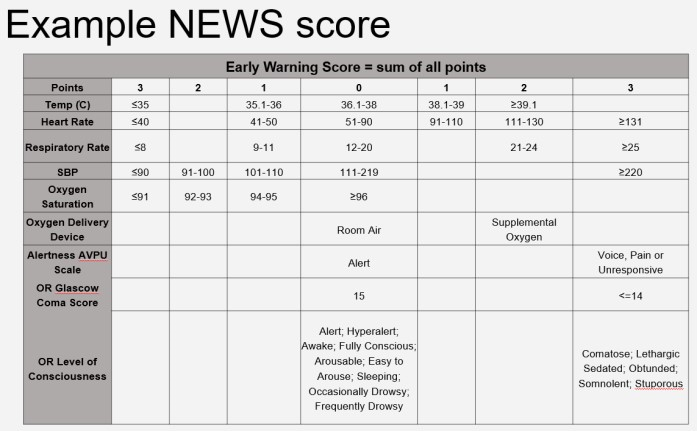
The technology that supports the ability to calculate the National Early Warning Score (NEWS) rests upon the foundation of the core EHR. The team configured core EHR solutions to automatically calculate each patient's NEWS and help care teams follow MU Health Care’s NEWS-driven nursing protocol. NEWS summarizes a patient's risk for clinical decline based on commonly tracked vital signs. The higher the NEWS, the more serious the patient's condition. The team decided to build the algorithm and to have the NEWS alert run in the background, without sending alerts, for two years. That allowed the team to fine-tune the algorithm and to provide proof to help justify the project's value. The growth in the algorithm resulted in 241 lines of step-by-step instructions that tell the computer how to respond to any information entered into a patient’s chart. It’s a list of if-then statements separated by “ANDs” and “ORs” that alerts the right people at the right time when a patient is deteriorating. And it does so without creating unnecessary extra work for the doctors and nurses caring for the patients.
The NEWS appears throughout a patient’s chart — in electronic flow sheets, care dashboards and physician and nursing handoff pages. Nursing unit leaders also monitor NEWS across their spans using nurse leader specific dashboards. Progression of the project over time allows scores that escalate into predetermined high-risk ranges to trigger a SmartZone alert (passive alerts within the physician workflow) for the patient’s provider and a Discern® or pop-up alert for his or her nurse. From the alert, the nurse launches a custom Elevated NEWS PowerForm to chart vital signs, review lab orders and results from the last 24 hours and even guides the nurse through what steps to take and which tests to order next.
The original timeline follows as below:
In 2020, the team added the PEWS score as well, so that all patient data have the capability of generating a score. They designed specific workflows for the general floors as well as for the Progressive Care units. The NEWS/PEWS do not trigger an alert for those patients who are comfort care only.
Workflows for the General Floor:
Source: University of Missouri Health Care

Source: University of Missouri Health Care
Workflows for the PCU:
Source: University of Missouri Health Care
Source: University of Missouri Health Care
The strength of the algorithm is driven by the physiological response of the patient as outlined in the below example. The NEWS team spent years running the algorithm in the background to refine the elements and the process. The alert had to be trusted, could not contribute to alert fatigue and any changes to documentation workflows had to be seamless.
Source: University of Missouri Health Care
When the NEWS is generated, the nurse will receive a pop-up alert within documentation as noted below and can launch directly into the designated next steps without signing into a different system.
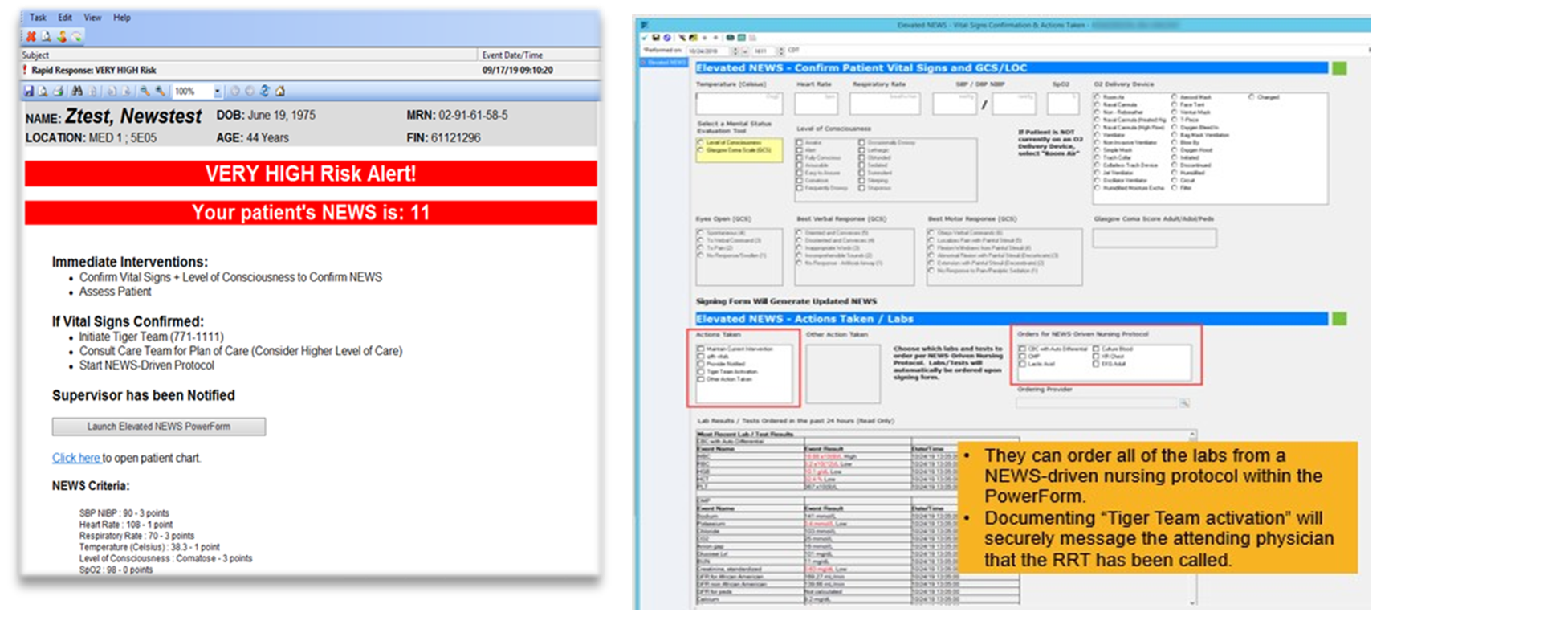
Source: University of Missouri Health Care
Providers are notified when the score is generated and the progression of care as the Tiger Team is notified for a rapid response event. While physicians do not receive these same Discern pop-up alerts for elevated NEWS scores, they do receive a less intrusive SmartZone notification within the patient's chart signaling that their NEWS is either High or Very High. Providers also will see the same kind of SmartZone notification in a patient's chart when a rapid response team has been called on the patient. By clicking on these alerts, the provider will automatically be taken to the results flowsheets within the patient's chart where they can see the vitals that triggered the alert, the actions documented by the nursing staff, and any interventions taken by the rapid response team.
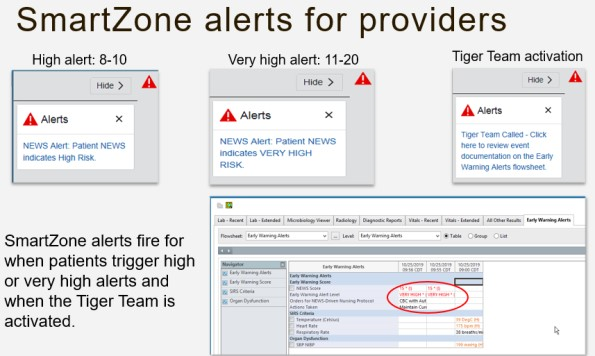
Source: University of Missouri Health Care
As noted below, NEWS can be displayed in the EHR, direct the care team to evidenced based next steps, and is also visible on near-real-time dashboards. Leveraging a truly integrated platform pushes the information in near-real time directly to the plan of care.
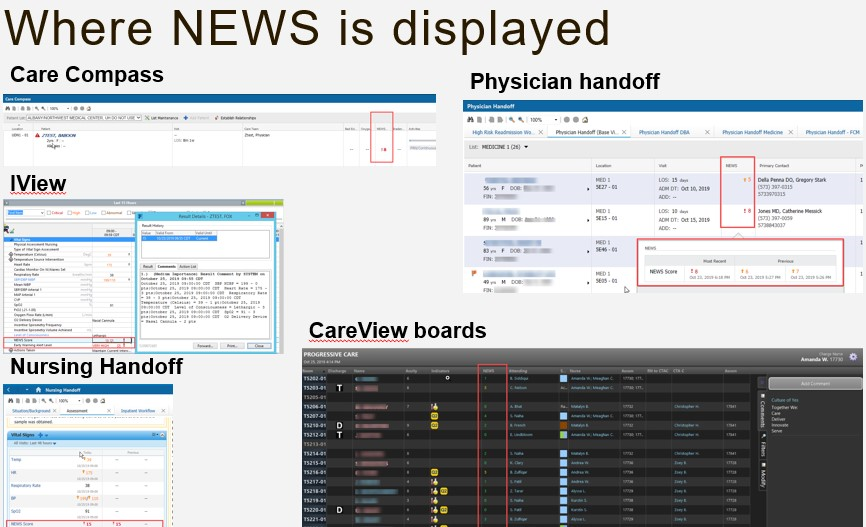
Source: University of Missouri Health Care
There are additional technologies that play a role in MU Health Care’s ability to impact surveillance and identification of patients in early deterioration. Point of care vital sign integration, bedside positive patient identification for lab specimens, order sets, and standardized care delivery, along with remote access to imaging such as ECGs, and X-rays also play a role in pushing key information to the care team both on-site and remotely. Providers also have access to a real-time documentation tool for Sepsis Bundle Compliance.
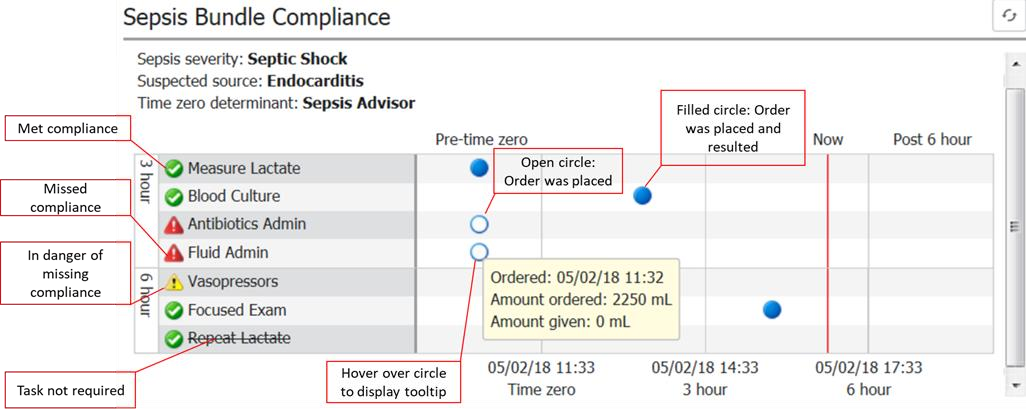
Source: University of Missouri Health Care
Improving Adherence to the Standard of Care
In 2017, the NEWS Leadership Team made the decision to generate a NEWS on all patients oldern than16 years of age. The NEWS alert algorithm ran in the background, without sending alerts, for two years. That allowed the team to fine-tune the algorithm and provided proof to help justify the project's value. With success proven in the adult population, in the spring/summer of 2020, they also began generating PEWS for patients younger than 16 years of age. Over time, the teams released the firing of the alerts for all patients (NEWS or PEWS) except those with comfort care only. Below are the definitions for inclusions, numerators and denominators, along with the adherence data supporting an improved outcome in overall mortality as well as in a subset of patients with sepsis. Outcomes will be addressed in the outcomes section.
Source: University of Missouri Health Care
Inclusion criteria: 100% of patients have a NEWS/PEWS score generated. Comfort care patients have a score, however, those patients do not generate an alert.
Studies show that early detection and rapid response intervention can have a positive impact on sepsis, as well as other patient conditions where a code blue or total cardiac and/or respiratory arrest are avoided. The NEWS Leadership team set a goal to increase rapid response team calls and to decrease the number of calls in response to a code blue. The evidence-based care guidelines built into the NEWS-driven nursing protocol ensures the organization has the capability to recognize and respond to a change in the patient’s condition. The Joint Commission does not call out rapid response teams as a requirement, however it is standard for a facility to have a process in place to recognize and respond to changes in a patient’s condition. The consistent utilization of NEWS / PEWS to monitor patients’ conditions, along with an increase in rapid response and decrease in code blue events in the light of improved severity adjusted mortality supports the current process, led to improvements in outcomes.
The following graphs indicate an adherence to the utilization of the NEWS / PEWS information as evidenced by increasing the rapid response team calls and decreasing the need to call a code blue. The numerator is respectfully, the number of Rapid Response Calls and the number of Code Blue calls. The denominator is respectfully comprised of all patients having a NEWS / PEWS score generated.
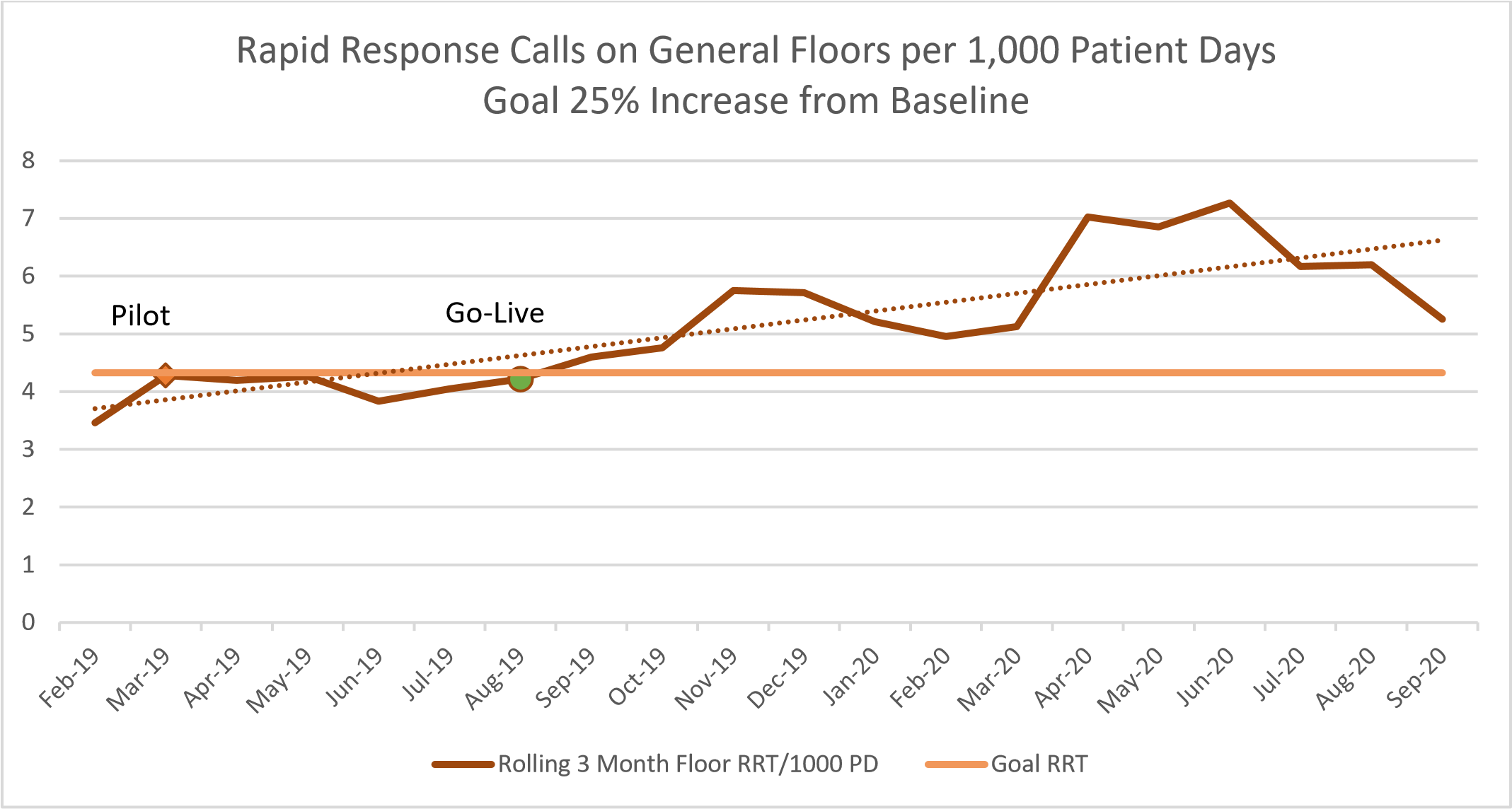
Source: University of Missouri Health Care
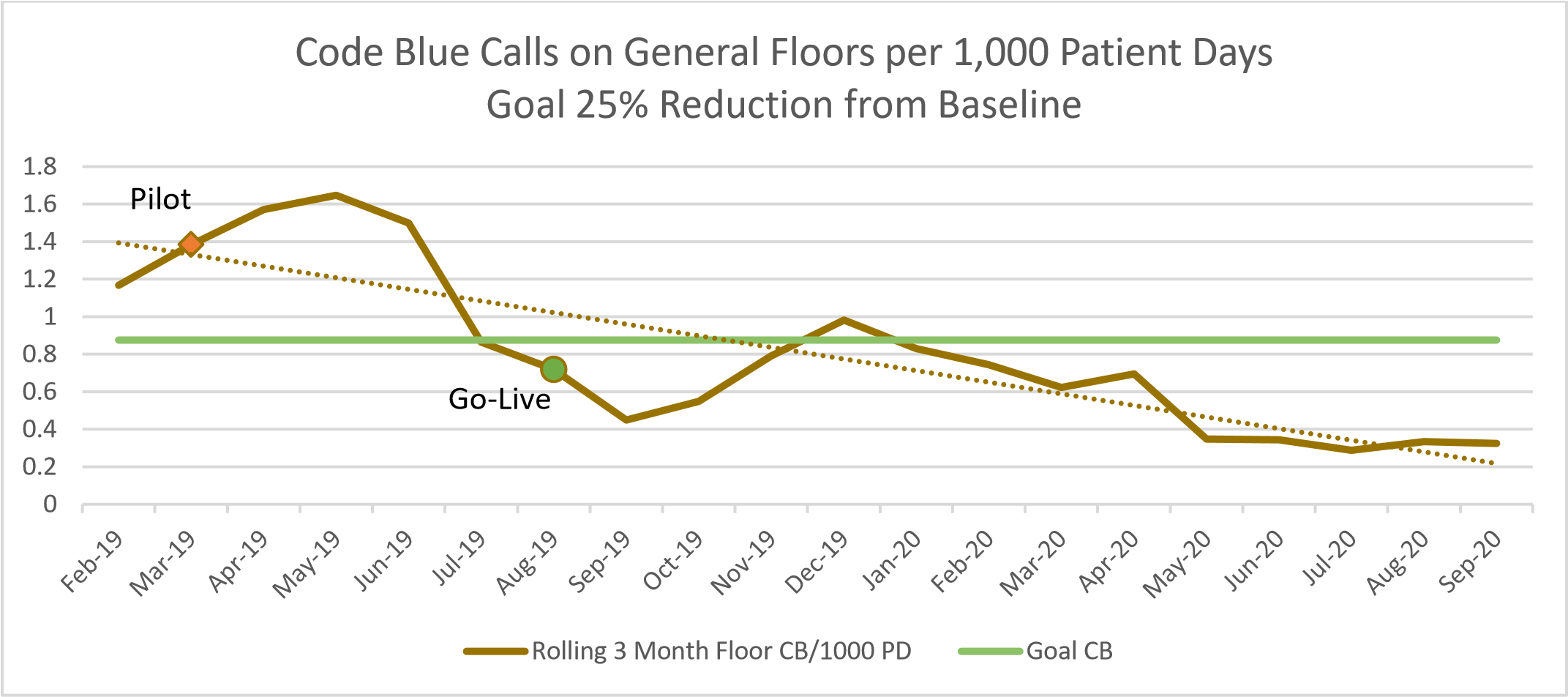
Source: University of Missouri Health Care
Improving Patient Outcomes
The pilot contributed to eight lives saved during Q2 2019 for the Internal Medicine Medical Service in the sepsis DRG. In the next few months, this grew to 12 lives saved. We also experienced an increase in the rapid response calls and a decrease in the code blue calls on the general floor. The pilot proved to be successful in the sepsis population. The team continued to improve the process and overall mortality also improved.
Sustained improvement in overall severity adjusted mortality.
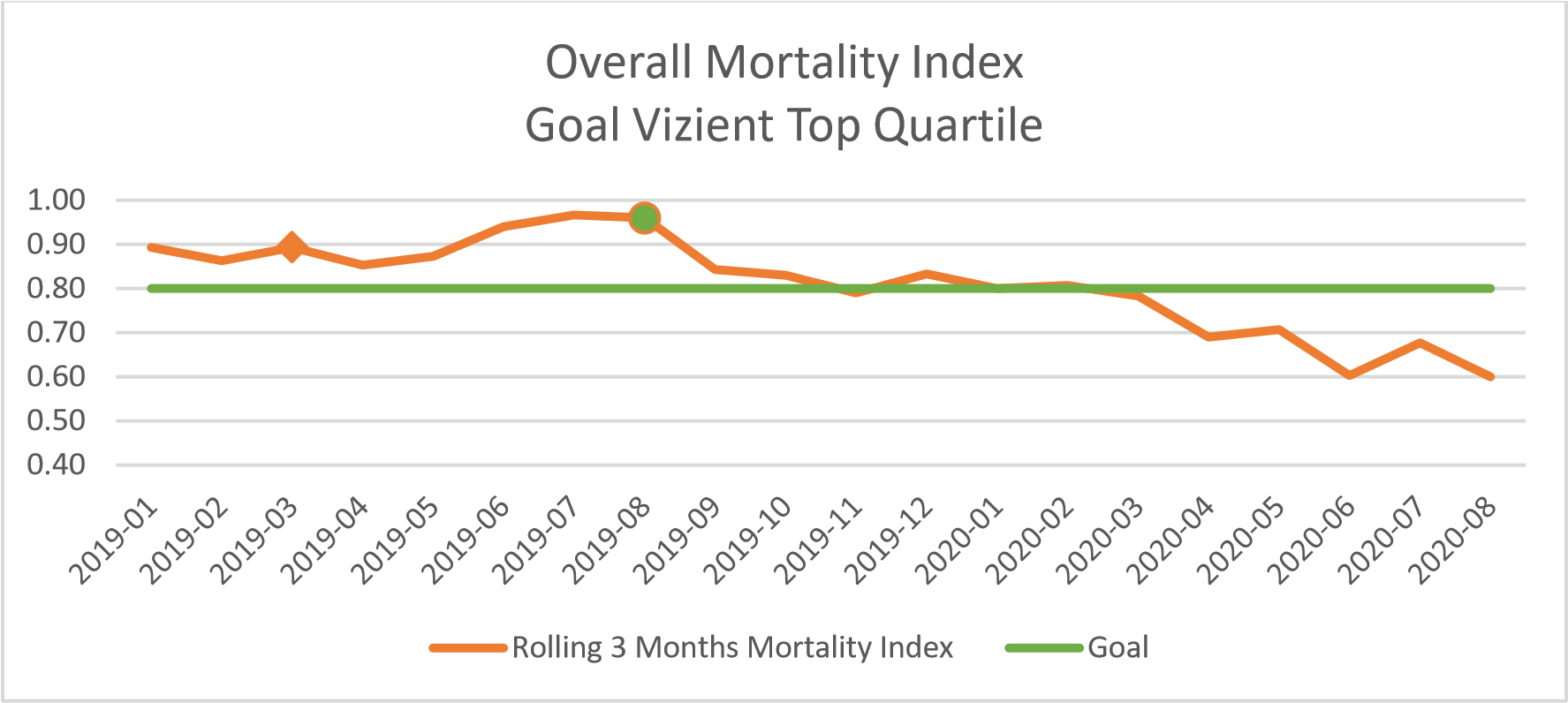
Source: University of Missouri Health Care
Accountability and Driving Resilient Care Redesign
MU Health Care uses the leadership dyad model, a model that promotes the pairing of a physician with a non-physician administrator for strategic and operational oversight. This model helps to drive accountability. If there is a deviation from the defined standard, there can be a one-on-one discussion, and the deviation can be discussed, studied and taken back to the Office of Clinical Effectiveness (OCE). If appropriate, the standard can be updated to reflect necessary changes. If the deviation from the standard is not appropriate, there are leadership councils in place to manage as needed. The same is true of nursing standards and the clinical informatics council working with nursing leadership when needed.
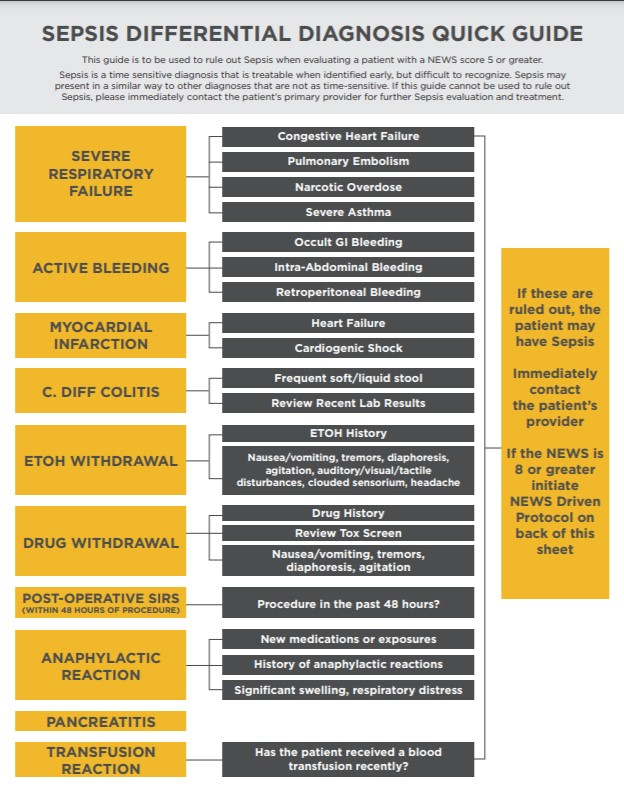
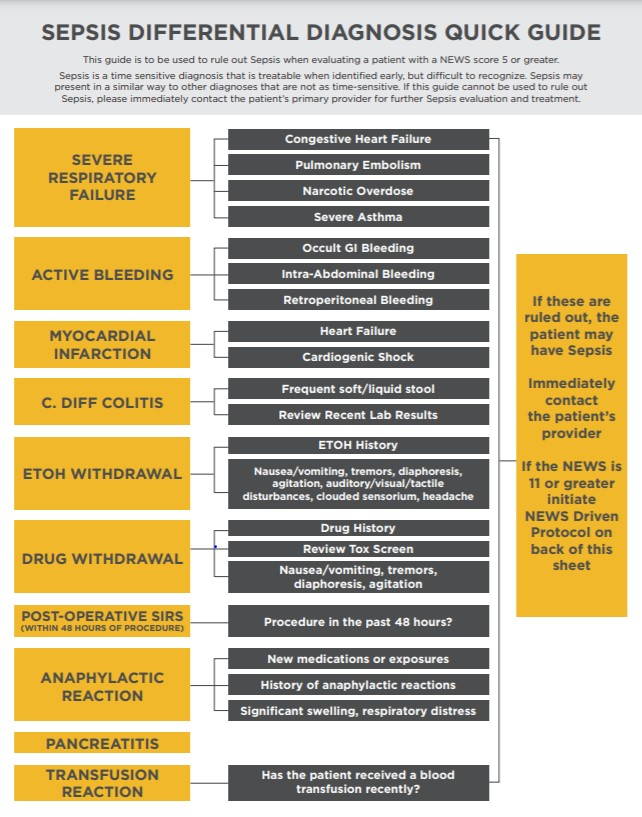
Data is always a driving force in innovative change. Along with the NEWS-Driven Nursing Protocol, a Sepsis Differential Diagnosis Quick Guide was developed to assist the rapid response team with ruling out sepsis when evaluating patients with elevated NEWS scores.
The data and tools utilized to imbed the NEWS has since led to the implementation of PEWS. MU Health Care took what it learned with the rapid response solution at the University Hospital and worked on both the Pediatric Sepsis Solution and the pediatric component of the Rapid Response solution concurrently (Pediatric Early Warning Score) to expand the capabilities of the Tiger Team to have an impact on rapid response activity in the pediatric space.
MU Health Care is a data-driven, data-governed organization. Teams have access to Vizient for benchmarking, a performance portal to gain insight into performance at levels from individual providers to the healthcare organization, and a real-time documentation Sepsis Compliance Bundle Tool.
The views and opinions expressed in this content or by commenters are those of the author and do not necessarily reflect the official policy or position of HIMSS or its affiliates.
HIMSS Davies Awards
The HIMSS Davies Award showcases the thoughtful application of health information and technology to substantially improve clinical care delivery, patient outcomes and population health.



